
When I read a book I have the habit of highlighting certain passages I find interesting or useful. After I finish the book I’ll type up those passages and put them into a note on my phone. I’ll keep them to comb through every so often so that I remember what that certain book was about. That’s what these are. So if I ever end up lending you a book, these are the sections that I’ve highlighted in that book. Enjoy!
Introduction
Asana – yoga postures.
Sthira – steady, still and firm foundation.
Sukha – good space.
At the most basic level, yoga postures increase our flexibility and strength. More subtly, they purify our tissues, and more subtly, they affect the energetic system the supports and sustains our tissues.
When all the moving and jumping is done, we can better sit comfortably and quietly without being distracted by our body. (Essentially, doing postures allows for a better meditation session)
Moving and jumping around is also a vehicle for studying the body in a deep and kinesthetic way.
If you haven’t done the exploration in your own body, it will be harder to lead someone though an exploration of theirs.
The body did not name its own parts. The body functions as a whole, rather than an assembly of individual parts.
Circumstances, decisions, accidents, and intentions all influence who we are. Every event in our life, from watching a movie to riding a bicycle or practicing yoga, has an influence on our being. Everything creates a wide array of informational energies that are absorbed by our system.
The general histories that make up a person are: Human Evolution, Genetic History, Learned Parental Behavior, Activities History, Injury History, Nutritional History, Spiritual History, and Mental/Emotional History. Look through all them when understanding where someone is coming from.
Sometimes we realize that we are turning into our parents, which we swore we would never do. It’s hard to escape the powerful imprints left by our parents during the formative years. We learn how to walk by watching and mirroring the way our parents walk. We talk, make expressions, and have similar body language as our parents. Our parents are the firs place we saw any of these things happening. In no way should we pass judgement on Mom and Dad. They did the best they could. It is our work to recognize the traits and behaviors that stem from our learned parental history and then determine which to maintain and which to discard.
In a large class situation, individuality is lost and everyone is given the same instruction.
Chapter 1: The Basics of Functional Anatomy
Connective tissues are comprised of two proteins – collagen and elastin. Collagen is known for its strength. Elastin is the more pliable and resilient stuff. Put them together in varying proportions and densities and you get connective tissue.
The denser and stronger the tissue, the more collagen is involved.
Ligaments and tendons are made up of a higher proportion of collagen fibers.
Ligaments are situated around the junction between two bones. You find them at joints or articulations. Ligaments lack a blood supply because they are packed together so densely, because of that they normally don’t heal when torn.
Tendons are the ends of muscles that attach to the bones.
There are 3 main divisions of fascia in the body:
- Superficial fascia – lies just under the skin and contains the fat cells that help maintain body temperature.
- Visceral fascia – surrounds and suspends the organs
- Deep fascia – surrounds all the muscles
The entire body is actually connected by this ubiquitous web of connective tissue.
The combination of fascia and muscle is referred to as myofascia. Myo = muscle, fascia = fascia.
There is no obvious end to a tendon as it weaves its way into the connective tissue layer around the bone. Ligaments also don’t have a clear starting or stopping point.
When connective tissue is freer, bones and posture shift into a more optimal position. Yoga can actively lengthen our connective tissues. As a result, we can realign our own skeleton.
Muscle is constructed of two types of proteins – actin and myosin. The basis of muscular contraction is that these proteins wait for the nervous system to send a signal to release calcium and cause them to become attracted to one another like magnets.
Muscle is made of layers and wrappings of fascia around proteins. So really, when you tear a muscle, you’re really tearing the connective tissue.
When you’re talking about lengthening a muscle in an asana, you are also talking about lengthening the fascia that’s surrounding it.
When lifting weights, the connective tissue has to adapt and change to the increased strength in the muscles. It does this by laying down new fibers of connective tissue and becoming denser, so that it can deal with the new amount of strength in that tissue.
Not enough movement means the connective tissue is not pressed to stretch and consequently tightens up.
When scar tissue is created, it can cause it to be glued together with the adjacent layer of fascia of the next muscle. This means a loss of independence of those two separate muscles.
Weaving its way into the muscular system is the nervous system, which tells the muscles what to do and how much tension to have.
As an example, the bicep’s action is to rotate the forearm so that the palm is facing up (supination) and to bend the elbow (flexion). But remember, All references to movements of flexion, extension, abduction, adduction, and rotation begin and end at the anatomical position. For example, normally the quads contract and straighten (extend) the knee by moving the lower leg. But in the back bend posture, instead of the lower leg moving the pelvis and femur move towards the lower leg at the knee joint.
There is normally one muscle that is the strongest in a particular action, but that doesn’t mean it’s the only one working. It’s more open-minded of us to look at the two ends of a muscle as attachments points.
Muscles contract. If they are going to create movement, one of the two ends will have to move towards the other (Or both towards one another). The one that is more stable will not move.
When a muscle contracts, not all the cells of that muscle are needed. The body determines how many cells to use based on past experience and current proprioceptive information.
When a cell within a muscle contracts, it contracts until it uses up all its energy (ATP).
If you do repetitions (like a bicep curl) eventually you will exhaust all the cells in the muscles involved. At that point, you will have exhausted all the ATP in that muscle.
Before the point of full exhaustion the mind/body knows to shift the responsibility from one cell to the next based on which cells still have energy. There is always a constant shifting of cells contracting within a muscle. This process continues as each muscle cell rests for a moment and rebuilds its level of ATP.
Muscles can shake when tensions occurs when one muscle tries to take us in one direction, and another muscle in a different direction.
Tonic contraction – The continual low-level muscle contraction that maintains our basic awake-but-resting posture.
Isometric contraction – When a muscle contracts but the overall length doesn’t change. (iso = same, metric = length). Basically when the bones are moving close to one another, or further away from one another.
There are two types of isotonic contractions:
- Concentric – The ends of the muscles get closer to one another during the contraction
- Eccentric – The muscles’s overall length increases with the contraction
The principle of opposing muscles states that when a muscle meets a resistance that it can’t overcome, its opposing muscle will relax. Basically, your body recognizes that it doesn’t want to add to that resistance. (Ex. when lengthening the triceps, if the biceps were to engage, this would add to the resistance you’re already pushing against.
An eccentric contraction of a muscle is the best time to stretch and lengthen it, because it’s not being asked to contract. For example, when doing a forward bend, instead of just eccentrically contracting the hamstring, if you concentrically contract the quad, in theory, because the quad contracts and meets resistance, the hamstring can relax and lengthen.
When doing a forward bend, are the hip flexors responsible for folding you forward? No, gravity and the weight of your upper body are responsible for the forward motion. technically, the hamstrings are responsible for controlling the movement into a forward bend.
When a muscle tear occurs, in order to make a strong connection so that the muscle itself can heal, the fibers are laid down in a cross-hatching type of pattern. The scar tissue goes against the flow of the torn fascia. Because of the added tension in the area, it becomes more likely that a subsequent inquiry will occur.
In the past, people would lie in bed for 4-6 weeks after surgery. Consequently they would lose range of motion. Doctors have found that rehabbing a patient sooner after surgery creates more scar tissue in the that’s organized in the original flow of the connective tissue. This leads to an overall quicker recovery time and better long-term mobility in the joint.
The above two points loop right into Peter Attia’s move as early as possible, as often as possible, as with as little pain as possible, and Joe Hippensteel’s never go above a 7 of 10 in pain when stretching, both of which make up my mentality about injuries.
Yoga seems to ultimately be about the nervous system.
Yoga is the cessation of the fluctuations of the mind. Loosely translated, yoga is a physical tool to control our wandering minds.
Golgi tendon organs measure the amount of force produced on the tendinous area where they are located. If a muscle over-contracts and nears the limits of causing a tear, the Golgi tendon reflex will occur, causing the muscle to relax in order to prevent injury.
For all movements, there is a response to the movement, whether it be a muscle contraction or release of certain hormones. Responses can be immediate or they can occur over time.
Activities we do regularly cause an almost unconscious melding together of the nervous and muscular systems in the body, known as facilitated pathways. What begins as a very conscious muscular action can evolve into a more unconscious muscular event. After doing certain activities over and over again, that information doesn’t even need to reach the brain for processing. Being relayed to the spinal cord and back is enough.
Facilitated pathways are even more observable on our mats when we stop moving and take a look at our postures.
Those of you with tight hips would have no problem doing a very nice leg-behind-the-head pose while under anesthesia (Unless bone structure is the cause of your inability.)
When students receive an adjustment or correction from the teacher, our mind may object, saying something like “That doesn’t feel right”. Really we’re just uncomfortable doing something outside the norm.
Ultimately, our work as yoga teachers is to help create a pattern that serves the student and their progression through the posture. The progression through the posture then relates to a progressive understanding of the student’s own body.
Keep in mind that is you are a teacher you will relate to your students through your own nervous system.
Really telling are the “preparations” that people make when they first sit on their mat before class has started. Are they rubbing their knees, their back, or their hips? Are they stretching certain areas of their body before they begin?
If you jumped up and down on one foot for a week without stopping, not only would you be extremely tired, but the bones in that leg would have become denser and, in a sense, stronger, as a result of all that jumping. Just as miraculous, if you would have never jumped up and down on that leg again, the density of the bones in that leg would return to roughly what it was before you started jumping.
Where would muscles attach if we removed the skeleton? How would muscles contract if we didn’t have a nervous system? How would we move if we didn’t have a muscular system? In this same way, we more deeply understand the importance of the skeletal system’s function in movement, where it almost always plays second fiddle to the muscular system. In terms of generating movement, one doesn’t do anything without the other.
Remember that the body has formed. The joint has also formed. It has formed in a particular shape, based on genetic coding as well as on stresses, stimuli, and input from other system and factors of development.
Chapter 2: The Foot and Ankle
The ankle is created by a bone that is part of the foot called the talus. The tibia (shin bone) sits right on top of it, with the smaller fibula off to the outside (lateral). The two bones create what is called a mortise, which basically looks like a monkey wrench. The shape is important because it limits how much side-to-side movement occurs at the joint.
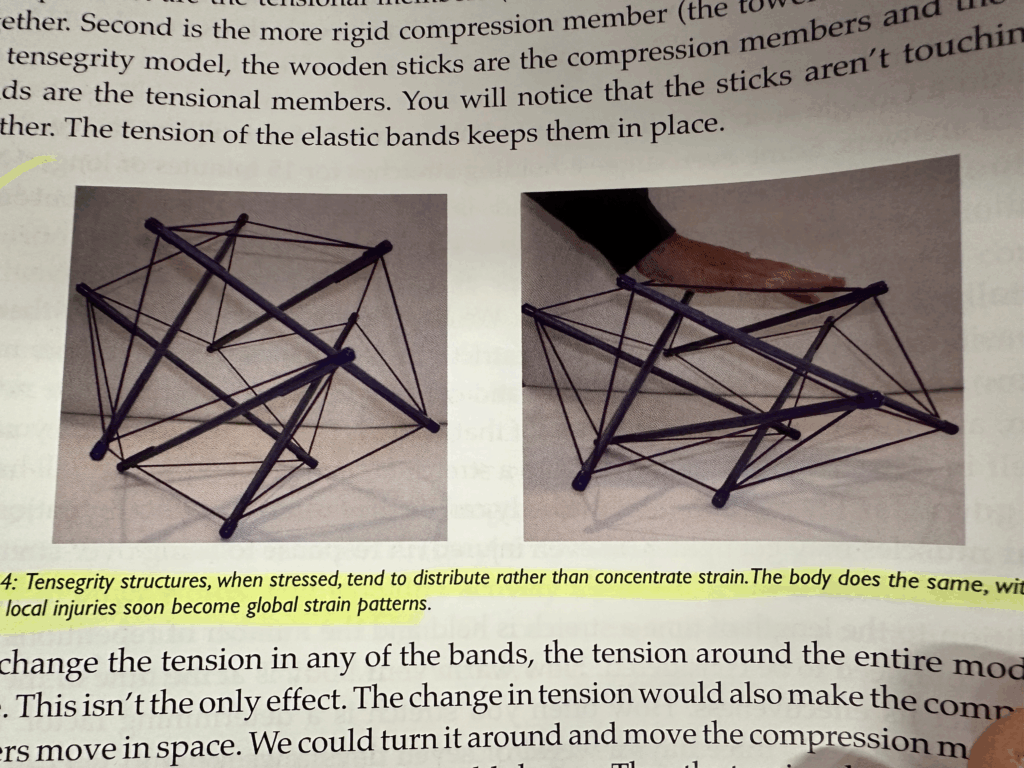
If we stand naturally, feet slightly apart, the forces of gravity pass through us in a straight line, whether we’re straight or not. If our bodies are in relatively good alignment, then that line flows through the body with few adjustments and compensations required by the tensional structures (tensegrity!).
The further our body moves away from this “perfect” alignment, however the more the tissues of the body will have to respond to maintain an upright position in relation to gravity. The stresses and strains of misaligned bones and tissues can lead to chronic pain.
The feet are similar to a foundation of a house. The foundation of a house must be even, otherwise the house will exhibit problems. Instead of forces running through the center of the beams, they may be running at slight angles.
As humans evolved, we lost the semi-opposable digit on our feet. This has brought our big toe closer to the second toe and shifted the way our weight travels through our feet. The center or axis of the foot now runs directly through the second toe. Most people have a second toe that is slightly longer than the big toe.
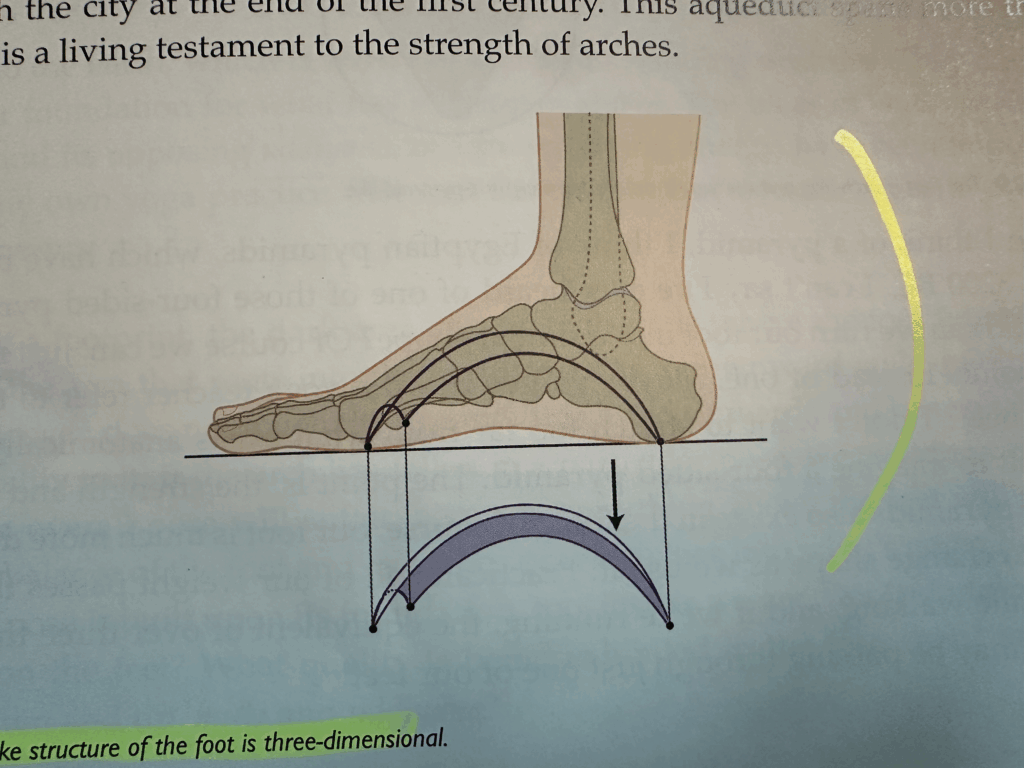
The most important evolution of the foot is the development of the arches.
The arch you see on the inside of the foot is the Medial Longitudinal arch. The arch on the outside of the foot is the Lateral Longitudinal arch. The arch that runs across the toes is the Transverse arch.
Although the second and third arches mentioned are not as obvious or critical as the medial arch, together they create an important synergistic quality.
If we’re running, the equivalent of over three times our body weight may be passing through just one of our feet.
It’s the bones that create the structure or shape of the arches in the foot.
The connective tissue and small bands of ligaments the tie the 26 bones together. If someone has a genetic disposition to loose connective tissue (hyper mobility), these little straps aren’t as tight as they should be. If the ligamentous band are more flexible, the bones more easily succumb to weight bearing and we end up with flat feet.
The bottom of the foot is the plantar surface.
Fascia is not as easily torn as a muscle but if you stand all day or if you run a marathon, then it can develop micro tears like overtime and that’s how it can lead to plantar fasciitis. Plantar fasciitis is essentially an enflamed plantar fascia.
The tissues in the medial arch of the foot act like the string on a bow & arrow (the arch is the bow part). They help maintain the distance between the ends of the foot. They also lift the arch by pulling the ends closer together.
One of the simplest ways we engage our arches in yoga is to lift our toes. Whenever the toes lift up, the tension in the plantar fascia is increased and the arches of the foot lift. As a result, the heel and the ball of the foot move closer to one another.
Although referring to particular muscles here, we’re always talking about a myofascial unit. The muscle is simply sophisticated connective tissue that has the ability to contract and relax. It’s important to remember the muscles ability to maintain a certain amount of tension.
The design of the lower leg (along with the forearm and hand) is such that the bulk of the muscle is placed above the part that moves. Think of how difficult the would be to move your foot around if you had large bulky muscles surrounding the joints. Instead, we have thin tendons the cross those joints to give it larger range of motion.
The ankle does 4 movements:
- Plantarflexion – moving the foot downward
- Dorsiflexion – moving the foot upward
- Supination – moving the foot outward
- Pronation – moving the foot inward
The one key difference between the two muscles in the posterior compartment of the foot is that the Gastrocnemius crosses both the knee joint and the ankle joint, where as the Soleus does not.
If the knee is flexed, the Gastrocnemius has less power to contract and extend the foot. When the knee is straight, you can’t bend the foot towards the shin as much than when the knee is bent. This is because the Soleus muscle contracts when the knee is straight.
Shin splits happen when the connective tissue layer around the bone known as the periosteum is pulled away from the bone itself and becomes inflamed. Overuse or strain of this muscle can lead to this condition.
If you were to stand up and balance on one foot, you would note that your foot continually corrects itself in a side-to-side movement, not forward and back.
The back of the leg is the Posterior Compartment, the front of the leg is the Anterior compartment, and the side of the leg is the Lateral Compartment.
Plantar Fasciitis is noticeable after a period of no use, often after sleeping. The first step out of bed after a night’s sleeps is usually intensely painful. It often subsides with movement.
The intense pain of Plantar Fasciitis after a period of no use is a result of scar tissue, which the body has created overnight. Splints are sometimes given to keep the plantar fascia stretched overnight as the scar tissue lays down. This way the next morning it doesn’t get torn again.
The source of Plantar Fasciitis is commonly the calf muscle, which connect to the plantar fascia via connective tissue of the heel bone. Of course, additional factors can create or exacerbate the problem too.
The relieve Plantar Fasciitis pain, stretching the gastrocnemius and soleus is often recommended.
Downward Dog and Forward Bends maintain length in the hamstrings, calves, and bottoms of the feet.
Without shock absorption (the plantar fascia) the shock is essentially sent back into the body and up through the knees, hips, and spine. Flat feet have been connected to a number of problems located far away from the feet, including headaches.
It is possible to rebuild the arches through physical therapy. In fact, many people experience significant gains in the health of their feet by practicing yoga.
- Forward bends stretch the calves as well as the hamstrings
- Chaturanga puts pressure on the toes, stretching the bottoms of the feet
- Upward Facing Dog stretches the tops of the feet while strengthening the opposite muscles on the bottoms of the feet.
- Down Dog also stretches the calves, and if you lift your toes, you increase the tension in the bottoms of the feet and strengthen the fronts of the shins
- Warrior 1 inverts the ankle and stretch and strengthens the inner and outer foot.
For Bunions, most people find that keeping the joints as mobile as possible helps. Instead of thinking what poses to do or avoid, think of consistently working with the feet.
Regarding ankle pain, it’s possible that the scar tissue over-accumulated and created adhesions. This make you more likely to re-twist your ankle because you have weakened the ligaments. Too much rest = more scar tissue.
Where you place your foot when bringing it into Half-Lotus pose is very important. If your hip is not flexible enough, the foot won’t land in the right place, and you’ll end up with more pressure exerted on the outer side of the ankle. The best way to alleviate ankle pain in Lotus is to back up and work on opening the hip.
Chapter 3: The Knee
Often when an injury occurs at the knee, there is some level of dysfunction at the foot and ankle joint below or the hip joint above.
To analyze the knee, you can look at kneecaps as “headlights” and observe where they’re shining their light.
The knee is the first joint to feel the effect of a fallen arch.
The underside of the patella has cartilage and thus easily and smoothly slides on the groove of the femur below.
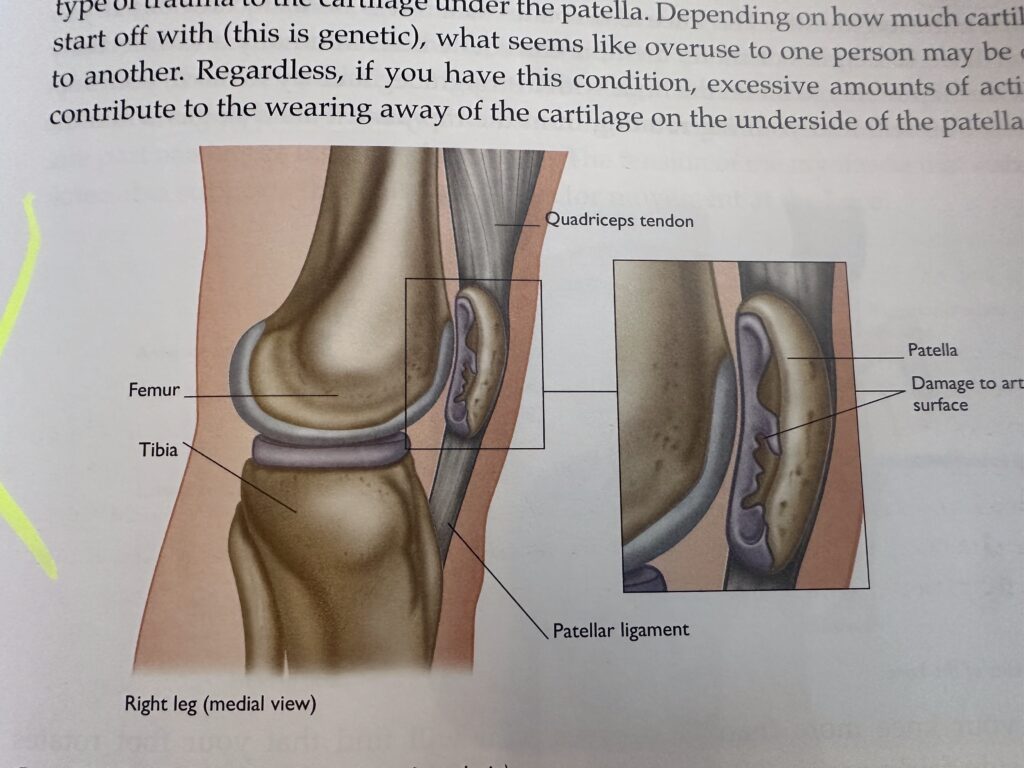
If the quadriceps on the inside (vastus medialis) is too tight, relative to the muscle on the outside (vastus lateralis), then the patella will naturally get pulled more medially. If this happens, there is more pressure on the medial part of the patella where it meets the surface of the femur. Tightness in the vastus lateralis would create the opposite effect. Either can lead to an uneven wearing of cartilage.
Ligaments allow for and restrict joint movements.
When the ligaments around a joint are in a “slackened” position, they allow for movement. When the ligaments become more “taut”, they restrict movement. In the knee, they are taut when the leg is in anatomical position (That is, extended or straight).
Ligaments play an important role in creating joint stability by restricting movement.
Two of the main ligaments of the knee are called the collateral ligaments. One is on the inside (medial) of the two bones and is thus called the medial collateral ligament or MCL for short. The other is on the outside (lateral) surface of the joint and is called the lateral collateral ligament or LCL.
The inside part of the knee tends to receive more stress.
The MCL is thicker than the LCL because it has more work to do in resisting stress and maintaining stability.
Cruciate literally means “crossing”. The two ligaments (ACL and PCL) cross one another. Unlike the collateral ligaments on the outside of the knee, the cruciates are on the inside of the knee. Anterior Cruciate Ligament = ACL, Posterior Cruciate Ligament = PCL. These strong ligaments are the primary stabilizers of the knee joint. They are taught when the knee is extended.
The ACL keeps the tibia from sliding forwards under the femur. It also prevents excessive medial (or inward) rotation of the flexed knee. There is a possibility the ACL can tear when the knee is flexed and either internally or externally rotated.
The PCL’s main purpose is to restrict the tibia from sliding backwards under the femur. In the cases when you do hear about PCL injuries, it often includes some type of hyperextension.
Ligament tears have 3 types:
- Grade 1 = Cause pain, but often no swelling or heat. Typically you just feel tenderness.
- Grade 2 = More significant pain and an increased amount of heat.
- Grade 3 = A complete tear of the ligament and would be associated with extreme pain, heat, and instant swelling.
When we go deeply into a ligament we find collagen molecules (proteins). A ligament is a huge bundle of these coils, just like a Slinky. A healthy ligament works in the same way as a Slinky. If you take the Slinky and uncoil it too much, when it springs back, there is a gap between some of the coils. This is either a Grade 1 or Grade 2 tear.
When an ACL is referred to as 50% torn, the ligament has lost 50% of its ability to stabilize the joint.
It’s common for the ACL to be torn when doing pizza while skiing and then catching an edge. The knee is bent while skiing and when it’s internally rotated and bent the ACL is put under high tension.
To repair an ACL tear, the surgeon takes a piece of ligament from another place or person and connects the ends of this “new” ligament to the places on the bone where the other ligament attaches. This is now your new ACL.
The 2 meniscus create a cup for the knobby ends of the femur to meet the relatively flat plateau of the tibia. This creates additional stability in the knee. They also play a shock absorber role in the knee joint. Instead of being completely fixed in place., the menisci actually move and distort in shap depending on the movements of the knee joint. Every time the knee flexes, the meniscus must slide or be “squished” backwards on top of the tibia to help keep those knobby ends in place. The opposite happens in extension. The meniscus slides or squishes forward. There is, in essence, a controlled sliding at the knee joint during these movements.
The medial meniscus is larger and more open at its center than the lateral meniscus.
The meniscus is designed to move with the bones. If it is compressed (For example, if the knee is completely flexed and then asked to rotate), the meniscus may be held down by the condyles and can stretch to the point of tearing. A similar thing can happen when the knee is moved very quickly.
One of the most common ways to tear a meniscus is to rotate a completely flexed knee. (Exactly what happens when we move into lotus)
Avascular = no blood supply.
The outer third of the meniscus maintains a blood supply and has the potential to heal.
Over time, small tears in the meniscus can get larger, be broken off, and float around in the knee. This is why common symptoms of a meniscus tear are pain, clicking, or locking of the knee.. When left alone, a tear usually progresses. Continued movement can cause uneven wearing of the cartilage surfaces on the bottom of the femur.
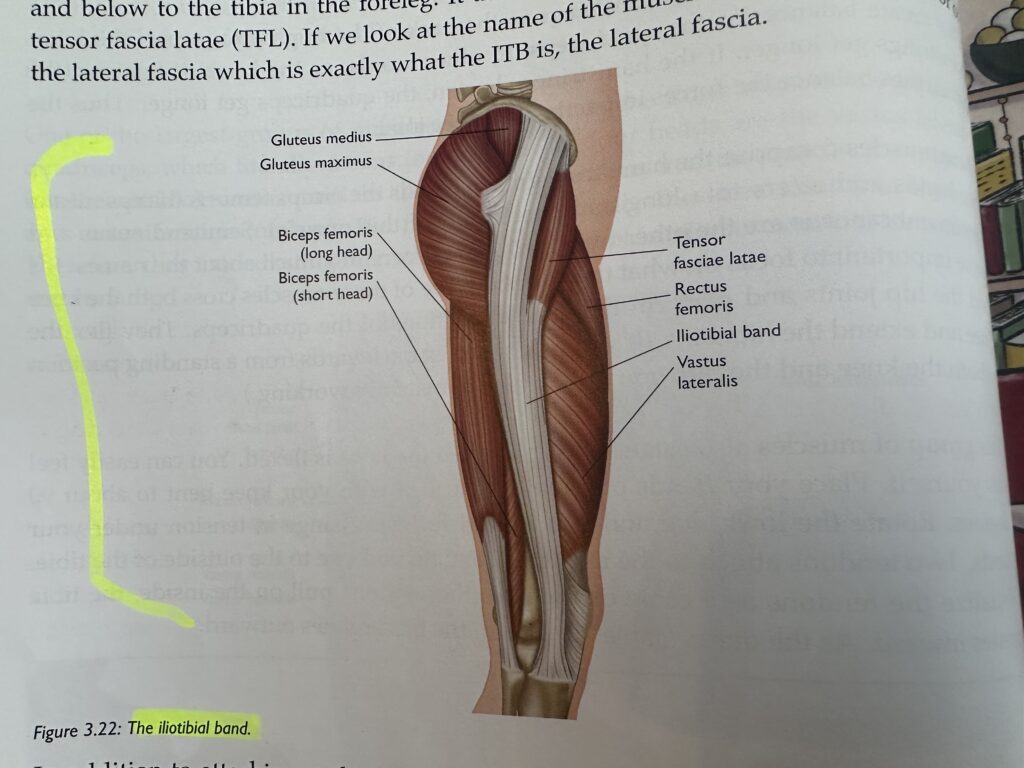
The IT Band is normally considered to be a stabilizer of the knee, especially during walking and running. With overuse, the IT Band can adhere fascially to the lateral quadriceps beneath it. Simply stretching it out with yoga postures may lead to trouble in other activities.
A loose IT band can cause instability while running. A tight IT Band can cause pain at the knee in postures like Lotus.
Bending the knees to transition between postures can be extremely helpful to students with SI, lower back, or knee problems. Once in the final pose, you should be trying to straighten the knees.
Take a look at your knee in a simple down dog and see where they point. Bend them slightly, and see if they point straight forward, inwards, or outwards. Better yet, lift your toes and see if this has any effect on your knees.
Step into Triangle Pose, and before you reach out to move into the posture, notice where your knee tends to point. If you bend the knee slightly, you’ll notice that it unlocks the hip and brings the knee to point straight forward over the foot.
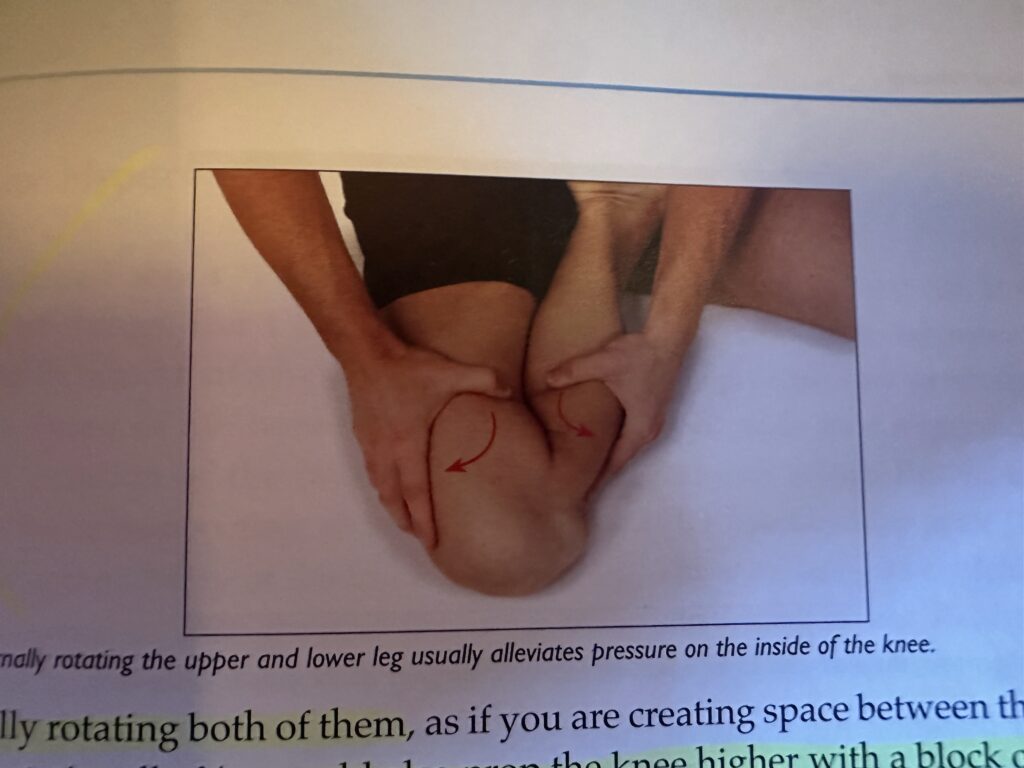
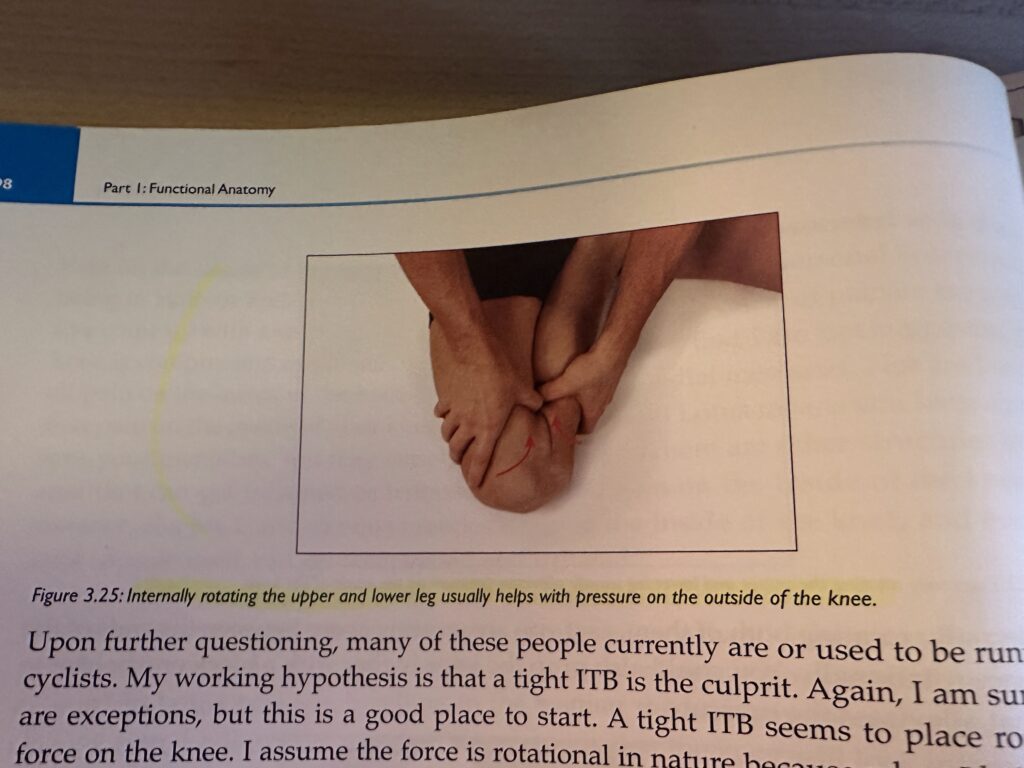
In Lotus, the moment you feel the sensation of pain, place one hand on your thigh near your knee and the other on your calf muscle. Try externally rotating both the thigh and the knee (below). You could also prop the knee higher with a block or bolster.
The long-term solution to getting rid of pain in the knee during lotus is to lengthen the tissues in the hip that are restricting external rotation of that joint.
Pain through the center of the knee in Hero’s pose is due to tight quadriceps. Elevate the pelvis so that the knee is not as deeply flexed.
In a hyperextended knee, the natural position of the bones requires less muscular effort. But, the tensegrity or supporting tension surrounding the joint is also gone.
Look at the knee’s ability to adapt and change through movement to diagnose issues. If someone is moving robotically through the legs, soften their knees a bit to help re-introduce the tensegrity of the knee. If they’re being soft in their knees statically, have them straighten their knees more and engage the quadriceps.
In Triangle pose, you will often find that the extended leg your are about to fold over is internally rotated. If you put a slight bend in the knee, you will find it then points straight ahead, aligning the two bones and the knee with the direction of movement.
Chapter 4: The Hip Joint
Where the ball of the femur meets the pelvis is the large depression called the acetabulum. If you look closely at the socket, you will notice that the top portion is like an overhang, but the bottom is open.
The hip joint is designed to support the upper body, including the spine.
On the surface of the acetabulum there is an additional piece of cartilage called the labrum. It functions much like the meniscus in the knee.
A labrum tear is often associated with pain and clicking in the hip joint, similar to what you find in a knee with a damaged meniscus.
Ligaments around the hip joint are particularly strong and dense. There are two in the front (iliofemoral and pubofemoral) and one in the back (ischiofemoral). Every movement is checked or restricted by at least one portion of these three ligaments. This joint is so stable that dislocations at the hip joint is quite uncommon.
The possible range or movement int he hip is tremendous – forward, backward, sideways, and it also rotates.
The most individual variation between people is found in the hips and shoulder.
Increases in the angle of acetabular antversion is normall associated with decreased joint stability. As yogis, however, an increased acetabular antversion could create a larger range of motion in the hip.
In a type 1 configuration of the hip, the head is almost a full sphere. Shafts of the femur are slender and the pelvis is generally smaller. Usually you get a greater range of motion and speed of movement.
In a type 2 configuration of the hip, the head of the femur is more like a half-moon and the shaft of the femur is thicker and the pelvis is larger and broader. The range of motion is decreased, but the joint is stronger.
With a joint that has the possibility to move at so many different angles, you must have muscles that can pull the femur in all of these directions too.It goes without saying that any of these muscles, if tight, can also limit the hip’s range of motion.
All four parts of the quadriceps group share the same distal attachment on the big bump located just below the kneecap.
3 of the quadriceps attach onto the femur, their function is dedicated to extending the knee. The 4th quardricep’s (rectus femoris) proximal attachment is on the front of the pelvis. Because it attaches onto the pelvis, it crosses the hip joint. The rectus femoris is capable of moving the pelvis into an anterior tilt. It’s also a two-joint muscle. Keep in mind that in two-joint muscles, the position of one joint affects the amount of tension through the muscle and thus impacts the other joint. The hamstrings are alos two-joint muscles.
the quadriceps can restrict our ability to posteriorly tilt the pelvis.
There are 3 muscles in the hamstring group. The three muscles cross the knee joint, two going to the inside, and one to the outside of the knee.
Two lesser-known functions of the hamstrings are internal and external rotation of the knee when the knee is bent at 10 degrees or more. the hamstrings also assist in rotating the hip joint internally and externally.
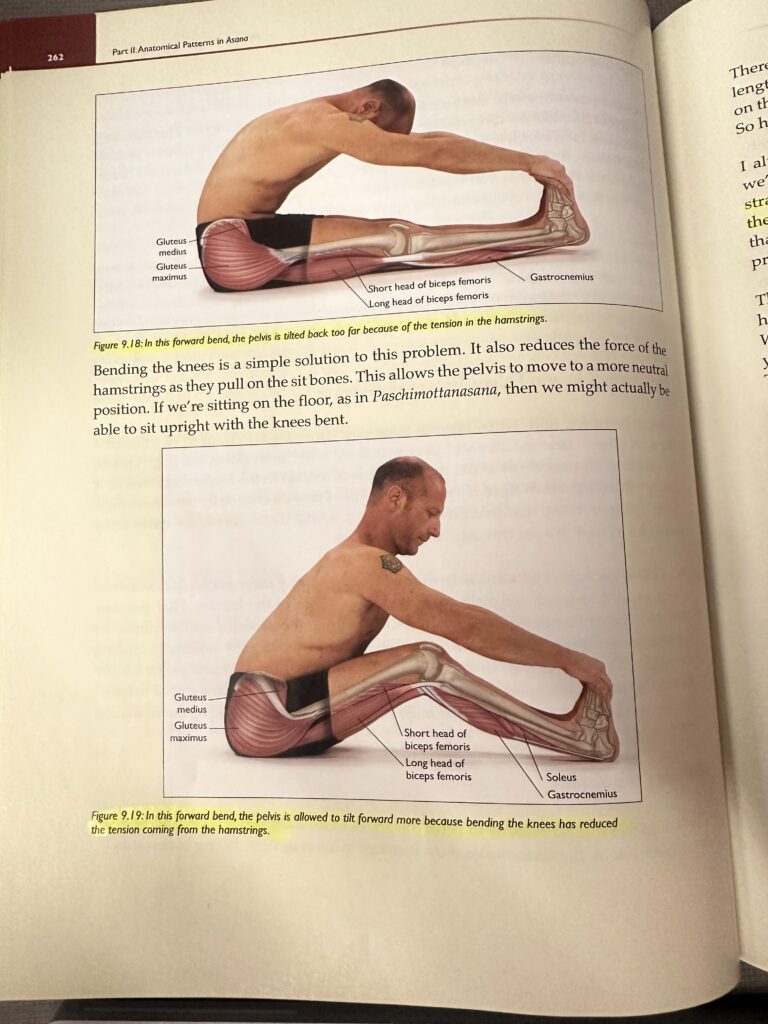
Bending the knees in forward bends shows how changing the tension at one joint (the knee) allows greater freedom at the second joint (the hip). These same muscles also restrict our ability to move our pelvis in an anterior tilt, as we can sometimes see in a Downward Facing Dog, where the pelvis is in a posterior tilt and the lower back is rounded.
the adductor group of muscles are flexors. Main purpose is of course adduction. These muscles attach onto the pubic bone and can pull down on the front of the pelvis and contribute to an anterior tilt.
We experience the limiting effects of the adductors as tension in the “groin”
In Warrior 2, the hip joint is both abducted and externally rotated. Yogis often look at how much tilt is in the pelvis in Warrior 2. The tighter the adductors, the more likely it is that the pelvis will tilt anteriorly (making the butt stick out.)
The attachment of the adductor magnus is far enough back that you often find the most posterior parts of this muscle function right along with the hamstrings in extending the hip.
The glutes work opposite the adductor muscles.
The gluetals prevent us from falling over by stabilizing the hip joint.
Large amounts of walking, running, cycling, and other activites that rely heavily on this repeated motion can create tight hips.
In any of these postures, a runner’s knee will commonly stick up at about a 45° angle.
The same muscle fibers that are so involved in walking and running also flex / extend and internally / externally rotate the hip. If the muscle is tight due to one of these repeated movements, it naturally influences the joint’s ability to do other movements.
The glueteus maximus extends and externally rotates the hip. It doesn’t assist in these actions until the demands are high enough. In regular walking, the glueteus maximus does not contract. Most people will naturally tighten the buttocks to help extend the hip joint when pushing up into a backbend. It supports the body weight and essentially keeps our hip from dropping too low.
The piriformis can create significant problems because of its relationship with the sciatic nerve. It can be easy to obscure the effects of the other deep six rotators on this area of the body or dismiss the possibility that something else is creating the problem.
The sciatic nerve normally runs under the piriformis muscle. If the piriformis muscle is tight, it can compress the sciatic nerve. This is the cause of sciatica. The other main cause of sciatica is compression of the nerves as they exit the vertebrae in the spine.
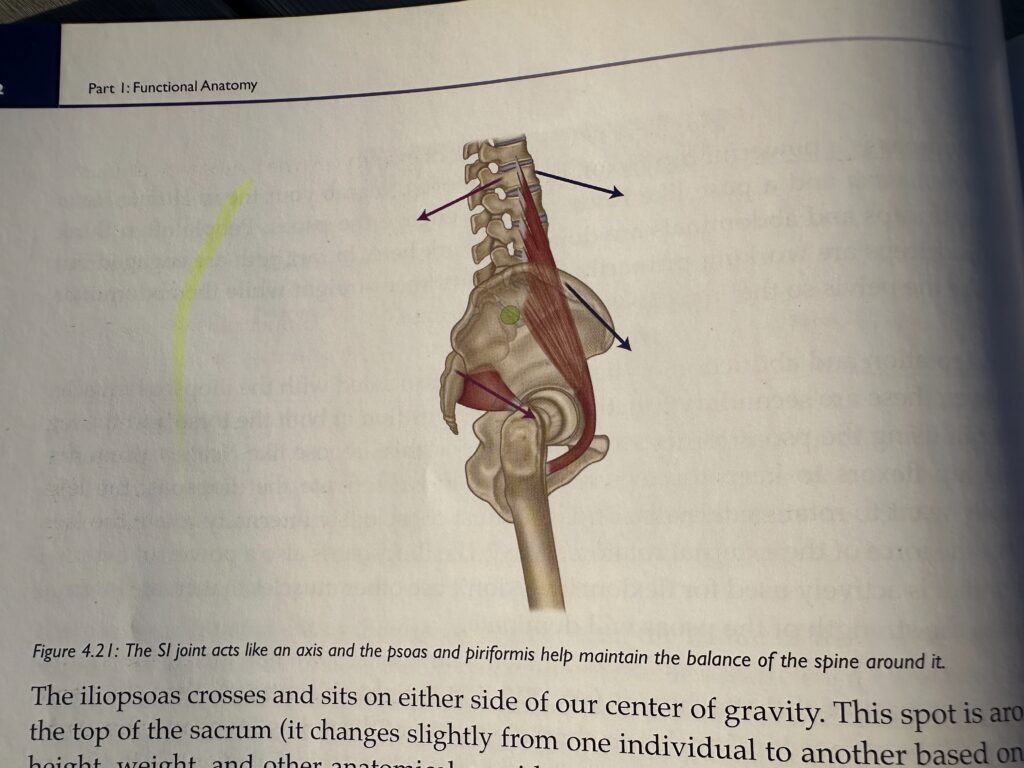
The tension of the piriformis pulls or holds the sacrum forward. Normally the piriformis helps maintain the position of the sacrum relative to the pelvis.
Normally if we do the opposite of a muscle’s primary action, we will stretch that muscle. However, if we’re not in anatomical position, that could change.
The Psoas is the single most important postural and structural muscle in the body and has a powerful effect on how you move. its functions are related to posture, movement, balance, breath, and energy. It crosses no fewer than nine joints on the journey from its proximal to distal attachments. If we intend to move in a way that is both strong and soft, both floaty and grounded, we must bring our attention to the psoas.
The psoas minor is present in perhaps half the human popular and is fairly insignificant for our discussion.
The iliacus and psoas major are often combined and called the iliopsoas muscle. Their distal ends merge together into one common tendon. they create the same action (flexion and external rotation) when they contract and shorten. When you hear the word psoas thrown around in a yoga context, people are generally talking about the psoas major.
Finger-like projections extend from the psoas major and attach onto the vertebrae. The muscle then sweeps down the sides of the spine and drapes over the front of the pubic bone and then attach to the femur.
The iliopsoas is also a powerful external rotator that is actively used for flexion. If we don’t use other muscles that create internal rotation, the strength of the psoas will dominate.
If the upper part of the attachment is tight, then the psoas would pull the upper lumbar/lower thoracic region of the spine down and forwards, creating less space between the lower ribs and the pelvis. If the lower portion of the muscle is tight or contracts, it pulls the lumbar region down and forward, creating an anterior tilt in the pelvis and a stronger lordotic curve.
The piriformis would pull the sacrum and coccyx forward towards the pubic bone, creating a force of counter-nutation on the SI joint. Because the psoas wrap over the pubic bone as it comes down from the spine, the tension is places on the SI joint via those vertebrae moves the coccyx backwards or away from the pubic bone. This causes the top of the sacrum to move forward.
If you want to move your center of gravity forward or backward, you’d better believe that hip flexion or extension is involved.
The iliopsoas is the functional core of our movement. When practicing we are either stabilizing or moving into and out of our postures. In order to maintain stability in a pose, the muscles closest to the center of gravity are the primary stabilizers. If we are moving, these same muscles are used to make the movement more efficient.
The iliopsoas does not function by itself, it takes the entire body.
Intentionally focusing on creating movements from your center of gravity of your body can be a major step forward in efficiency of movement.
The pelvic floor and the base of the spine both represent the roots of our energetics. The root chakra deals with survival, self-preservation, stability, groundedness, and trust. Mula bandha is associated with preventing the escape of energy through the bottom of the pelvis. Uddiyana bandha brings the element of lightness, an upward flying from the roots that have been established. Watching an advanced yogi moving with lightness of limb illustrates that we must access energy, not just physical strength to move in this way.
The position of the leg in Warrior 1 is an example of isometric contraction. In Warriro 1, the gluetals and hamstrings (hip extenders) also work to prevent further flexion at the hip joint. These muscles keep the hips from sinking further towards the floor.
A year of bent-knee forward bends can create hamstrings where the distal end becomes too tight. It’s okay to start this way to lengthen the hamstrings, but continuing to do it for too long can cause problems.
The deep six rotators and the gluteus minimus and medius are the key culprits restricting access to Lotus Pose.
The movement back from Uttanasana to High Plank is an extension of the hips. The returning jump forward is flexion of the hips. What is moving through the air is the center of gravity.
Changing the tension of the quadriceps (and thus the tension of all the joints it affects) in a short amount of time is not a good idea.
Any strong extension of the hip joint should stretch the psoas. Lunges are a great one.
Chapter 5: The Pelvis
The bones that comprise each side of the Pelvis become completely fused during puberty. That’s about how long it takes for the fusing to complete.
The female pelvis tends to be slightly wider, the acetabulum faces slightly more forward than in men.
The ASIS (Anterior inferior iliac spine) is in front and PSIS (Posterior superior iliac spine) in back. If we draw a line between these two points and measure the angle, in most men the line sits at 0 degrees.
Because the pelvis is connected to the sacrum, movements of the pelvis also lead to movements in the sacrum or spine.
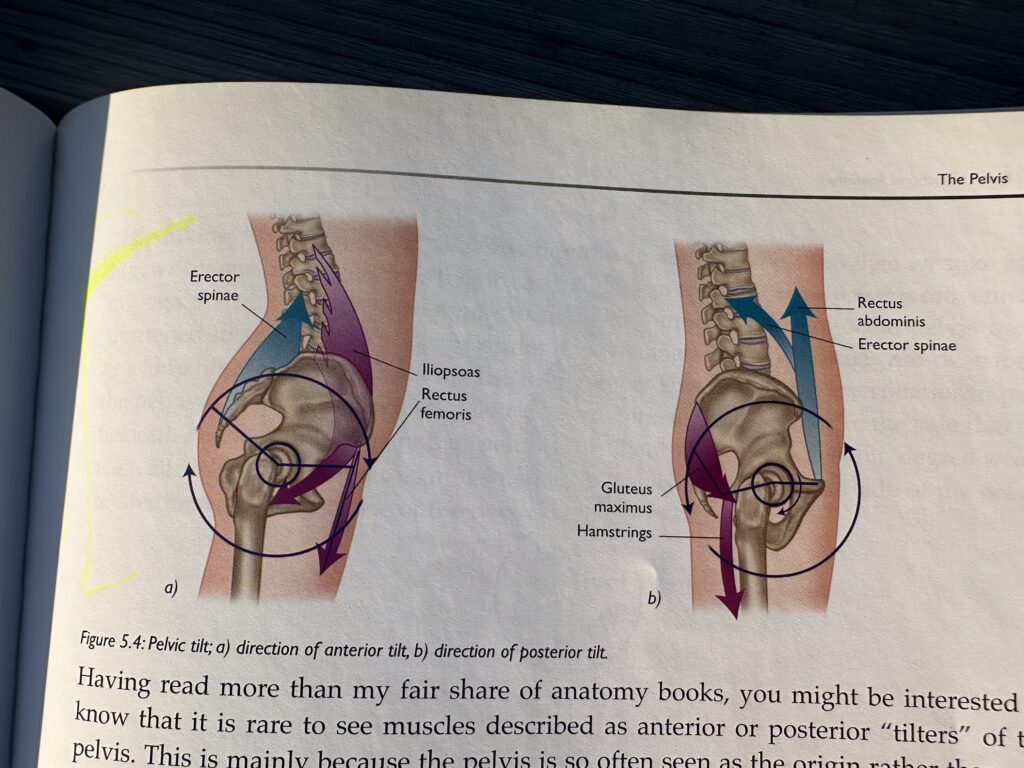
Think of the pelvis as a pulley wheel that moves around one axis and can spin in either direction, depending on where the forces is coming from. Pulling on it from the front and belo wil cause the same rotation as pulling on it from the back and above.
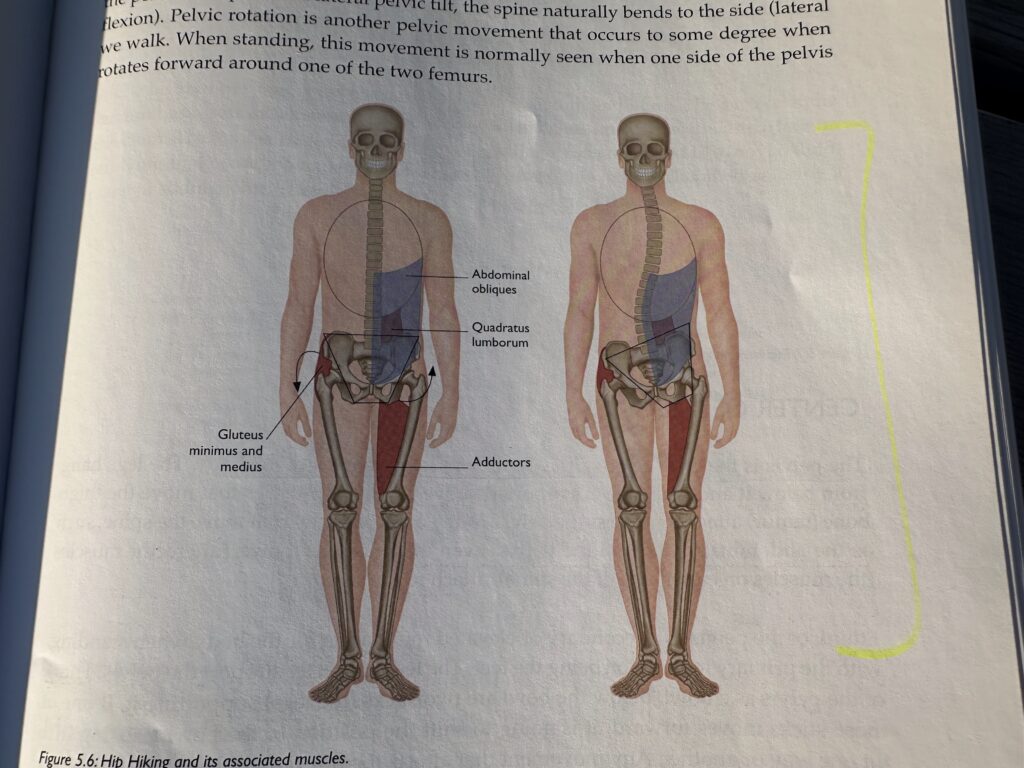
In Revolved Triangle, not only does the right hip tend to move closer to the ribs, but the left side of the pelvis also tends to drop down.
Think of the pelvis as a bowl. Below the bowl are two sticks (the legs) supporting it. If one of those sticks moves forward, it is going to shift the position of the bowl.
The average person has, at most, a few millimeters of movement at the SI joint. Some might have none at all.
If you engage the levator ani muscle group, the contraction is not limited to the muscles of the pelvic floor. There is also a corresponding contraction in the lower abdomen.
Depending on the individual and the tension in their hips, the foot placement may have more or less of an effect on the pelvis.
If the pelvis is not straight or square relative to the feet, then the spine must compensate. Where the spine goes, so goes the head, and slowly everything must rearrange itself using muscles and tension in ways that aren’t necessary.
If the pelvis can’t rotate freely over the heads of the femurs (usually because of tight hamstrings), then the spine is more likely to become part of the forward bend.
As teachers, keep in mind what we are looking for – We’re looking for the muscles that are not allowing a particular movement to happen.
In forward bends, the forces of the hamstrings prevents movement of the sit bones, and thus, the rest of the pelvis. In fact, their tension actually pulls the pelvis in the opposite direction from where it wants to go naturally.
To prevent counter-nutation, get your pelvis to move in the same direction as the sacrum.
If you can posteriorly tilt your pelvis, or reduce the amount of anterior tilt it creates from the beginning, you will reduce the amount of pressure at the SI joint. We are often told to tuck our tailbone – most people respond by squeezing the buttocks. This actually ends up adding extension to the hip joint and increases the pressure of the hip flexors (not ideal).
SI joint movement is certainly important (when addressing SI joint dysfunctions for example), just not in terms of increasing range of motion in backbends.
During pregnancy, hormones are released that soften the ligaments around the pelvis for childbirth. The SI joint moves more than it normally does. This is good for childbirth, but if the ligaments are overstretched, they may not return to their “normal” amount of tension.
The movement that is most likely to irritate the SI joint is twisting.
If you are doing a seated twist, allow more of the twist to happen at your hip joint; do not over-twist through the lumbar spine, which naturally puts more pressure into the SI joint.
In Mula Bandha, think of the bottom of the pelvis as a trampoline of layered tissues.
The purpose of mula bandha is to prevent the escape or downward movement of energy through tyhe pelvic floor.
The breath is the prana, or life force, that animates our physcial bodies. When the diaphragm contracts (on an inhale), it compresses the abdominal contents and puts a downward pressure on the pelvic floor. By contracting the pelvic floor muscles, you prevent the downward movement of these muscles when breathing. In addition to stopping the downward flow of energy, you are literally stopping a downard physical force.
Mula bandha is the root lock. Uddiyana means upward flying and is and overall ease and a particular lightness in the practice. The very famous, floating aspect in advanced practitioners is a sign of bandha use and control.
A full uddiyana bandha is not possible when breathing. A full uddiyana is done on a held breath during pranayama and is known as a kumbhaka. During asana practice, if you are performing uddiyana, you are doing sort of “half” uddiyana.
The psoas is located in the root chakra area and has the ability to create the lightness that we’re talking about. Awareness of an ability to use the psoas seems to trigger the resultant effect of uddiyana bandha.
How many of us had trouble preventing our pelvis from sagging when we first started jumping back? With a strong psoas muscle, the hip joint itself and the pelvis are stabilized. To get our feet between our hands we need to flex the hip joints. What does this better than the psoas? Because we are essentially “in the air” while this is happening, it is pure hip flexion versus hip extension.
This combination of functional movements while controlling your center of gravity is very powerful. Add to this a stable foundation through the hands and the shoulders and you will find a slow and controlled movement that fits the expression of being both grounded and light.
The mula bandha refers to the root lock, which is associated with the pelvic floor. Its purpose is to prevent the downward flow and escape of energy through the bottom of our torso. Uddiyana bandha is translated as “upward flying” and is the energetic lock responsible for the lightness we see in an advanced yogi’s practice. The main muscle of respiration (breathing) is the diaphragm.
The diaphragm attaches in its posterior part onto the spine and then circles around to the bottom of the rib cage.
On our belly breath, the top of the diaphragm isn’t moving down much more than an inch, if that much. The heart is sitting on top and is connected to the diaphragm moved down too far, what would happen to the heart? As it surface moves down, it pulls on the connective tissue bags that surround the lungs. As a result, negative pressure is created in the chest cavity and the lungs fill. At the very end of inhalation, you may feel a light pressure on your pelvic floor as it stretches or is pressed down by the abdominal contents.
Tightening the pelvic floor means that when pressure comes down from the contracted diaphragm, it won’t push the tissues at the base of the body downwards. The tension of our contraction prevents it. This is the purpose of mula bandha. It prevents the downward movement of energy. In this case, we prevent the literal downward movement of the pelvic floor.
When we pull the lower abdomen in and hold it there during both inhalation and exhalation, the diaphragm no longer has the ability to push down and the abdomen is restricted from moving out. The force gets redirected upwards into the chest. This is the purpose of uddiyana – to direct the energy / breath / prana upwards.
If you take a big breath, the abdomen are pressed outwards. If you tense the muscles of thye pelvic floor and abdomen to prevent them from going out (as one does when applying mula and uddiayana bandhas), then the diaphragm functions differently. The breath is re-directed upward.
Creating mula and uddiyana during asanas physically changes the way our breathing happens. This mirrors the energetic intentions of the bandhas, one of which is to provide us with a focal point in our practice that will support the body. When we engage the bandhas, we also contract the muscles that help us integrate movement and stabilize our spine.
If the intercostal muscles are tight, they will restrict the movement between the ribs.
It’s most difficult to breathe in backbends and twists. During those, pressure is being placed on the ribs and the tissues. If you can’t separate the ribs from one another, how will the lungs be able to fill inside of the rib cage?
Yoga always shows us where to focus and where we need to work. It is at the edge of our comfort zone that change is created. When we arrive there with the breath, and then breathe.
Chapter 6: The Spine
The discs in the spin are fluid-filled discs of cartilage that provide shock absorption.
The overall health of the spine and associated discs is intimately related to how much pressure the various tissues surrounding the spine place on the vertebrae.
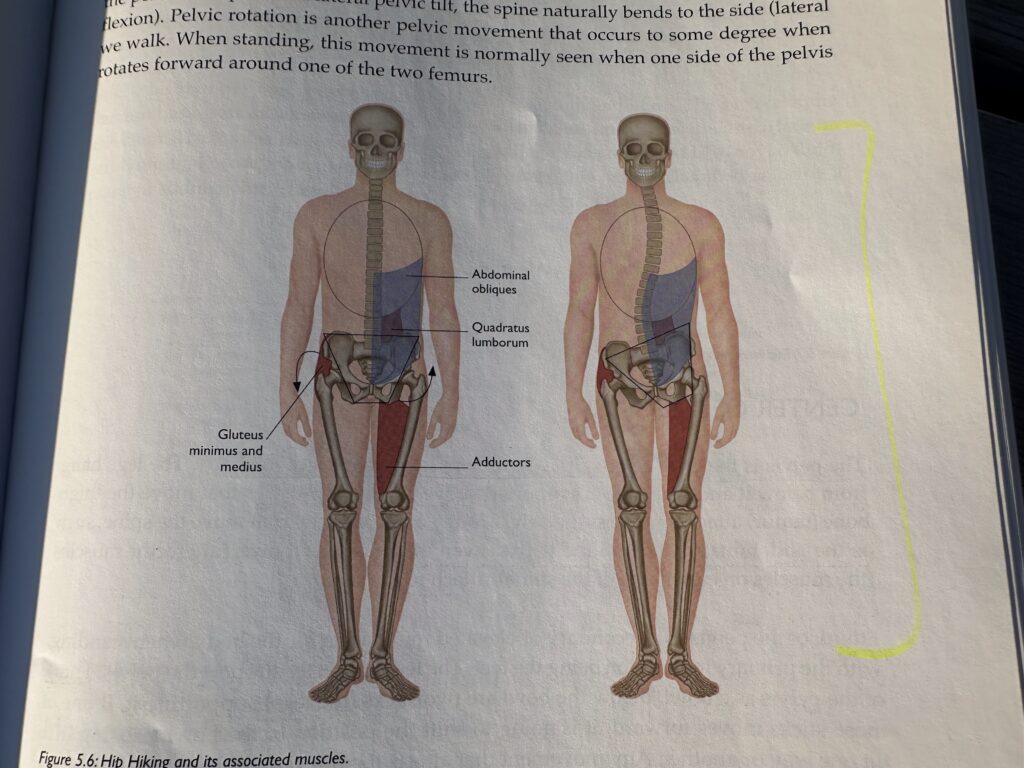
The curves in the spin are important and add 10x more strength to the whole structure than if the spine was truly a column.
If the pelvis is off kilter, it puts pressure on the sacrum, thereby forcing it off at an angle. When this happens, the spine naturally tries to correct itself to keep the head and eyes even with the horizon.
The lower you go on the spine, the larger the vertebrae in order to support the vertebrate above.
L4 and L5 are at such an extreme angle that they actually have extra ligaments on their posterior part that attaches to the pelvis. These are called the iliolumbar ligaments and are an extra support mechanism for keeping these vertebrae in place.
In the T12 area of the spine, there is marked change in the range of function as there is less need for size because weight-bearing is reduced.
When sidebending, on the opposite side, the flexibility of the intercostal muscles will help to determine how far apart the ribs can go from one another.
C1 = Atlas, C2 = Axis
All of the muscles of the back at the same depth share a similar goal: to maintain the spine in an upright and erect position.
Three muscles comprise the erector spinae group. These muscles activate around the spine when doing backbending postures.
Tissues that form the abdominal cavity also affect the spine. These are the abdominals and have three layers. The most superficial is the external oblique, which lies on top of the internal oblique. Beneath these is the transverse abdominis.
The abdominals attach along the bottom of the rib cage. They then head down to the top of the pelvis. Because of their attachment points, the abdominals (though far away from the spine) both stabilize and move it. All three layers assist in flexing the spine as they pull the ribs down towards the pubic bone.
When a muscle has the ability to create a movement, it also has the ability to restrict a movement.
The abdominals also have the abiliyt to move the pelvis. If the rib cage is sufficiently stabilized, the pubic bone can be lifted upwards, creating a posterior tilt of the pelvis. this is common instruction given in Utkatasana or Virabhadrasana II.
The spinal discs are most filled with fluid in the morning. Due to a process called disc imbibition (by which the fluid inside the disc is absorbed into the surrounding bones throughout the day and then re-absorbed back into the disc itself when at rest, like during sleep).
During normal activities such as walking and sitting, pressure is placed on the discs and the fluid slowly seeps into the bones. When we go to sleep, pressure is removed from the discs, adn the fluid then seeps back into them. The more fluid you have in the discs, the stronger they are, due to the increased pressure moving outwards against the cartilaginous wall.
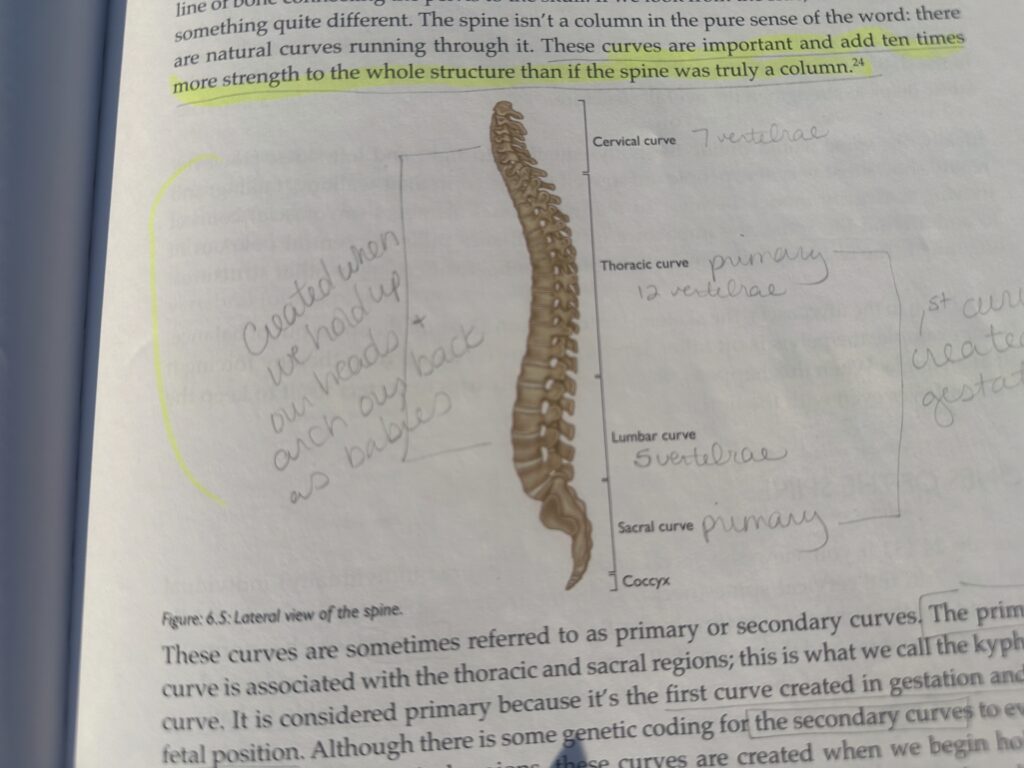
The discs in the spine act as a space. The nerve roots that come out of the spine require a certain distance to be maintained between the two vertebrae.
The overall function and maintenance of tensegrity in the spine is due to opposing forces. The discs are naturally pushing while the ligaments are inherently pulling.
Just because a disc is bulging does not necessarily mean that it will cause pain. If the disc sticks out far enough to press on the nerve root, it will cause sensation further down that nerve.
For a herniated disc, one part or area of the disc is weakened. The fluid of the nucleus pushes the weakened section out further than it normally goes.
A common response from the body when certain types of injuries happen is to try and splint that area to prevent more movement. If the splinting continues beyond a few days, it starts to cause a lack of blood flow in the tissues that are splinting.
in a ruptured disc, the cartilaginous ring or disc itself tears from its outer wall to the center, where the nucleus and fluid are. the fluid then leaks out from the disc. The space between the bones is reduced.
To fix a ruptured disc, surgeons take metal hardware and bolt the vertebrae together so that the space between them is maintained. the problem with fusing the vertebrae together is that you create a kink in the chain of movement running through the spine. If there are two links in the middle of that chain that don’t move, you have a new place for stress to build.
Chapter 7: Comparing the Upper and Lower Extremities
The socket for the femur is much deeper than the one for the humerus. The femur is built to handle weight and movement while the shoulder is built for mobility.
3 bones come together to create the shoulder girdle. The upper arm bone (humerus), the shoulder blade (scapula), and collarbone (clavicle).
In the pelvic girdle, the scapula and clavicle are not attached to the stable structure of the spine via the sacrum. The clavicles attach to the sternum but they are much more free to move around than their counterparts in the pelvis.
The end of the clavicle attaches to the sternum – the only place that a bone from the shoulder girdle attached to the axial skeleton. A small cartilaginous disc between the sternum and clavicle helps mitigate the forces that naturally run through it. There’s not very much movement at all at this juncture. If these ligaments tear, we have “separated shoulder”.
The scapula (shoulder blade) itself does not sit flat on the back. The rib cage is more round and if anything the scapula sits at about a 45-degree angle relative to the body’s orientation.
The shoulder blade slides around towards the front of the rib cage and also slides back so that the two scapulae move closer to each other on your back. This is called protraction and retraction.
The bottom tip of the scapula is called the inferior angle.
Unlike the scapula, the clavicle can also rotate.
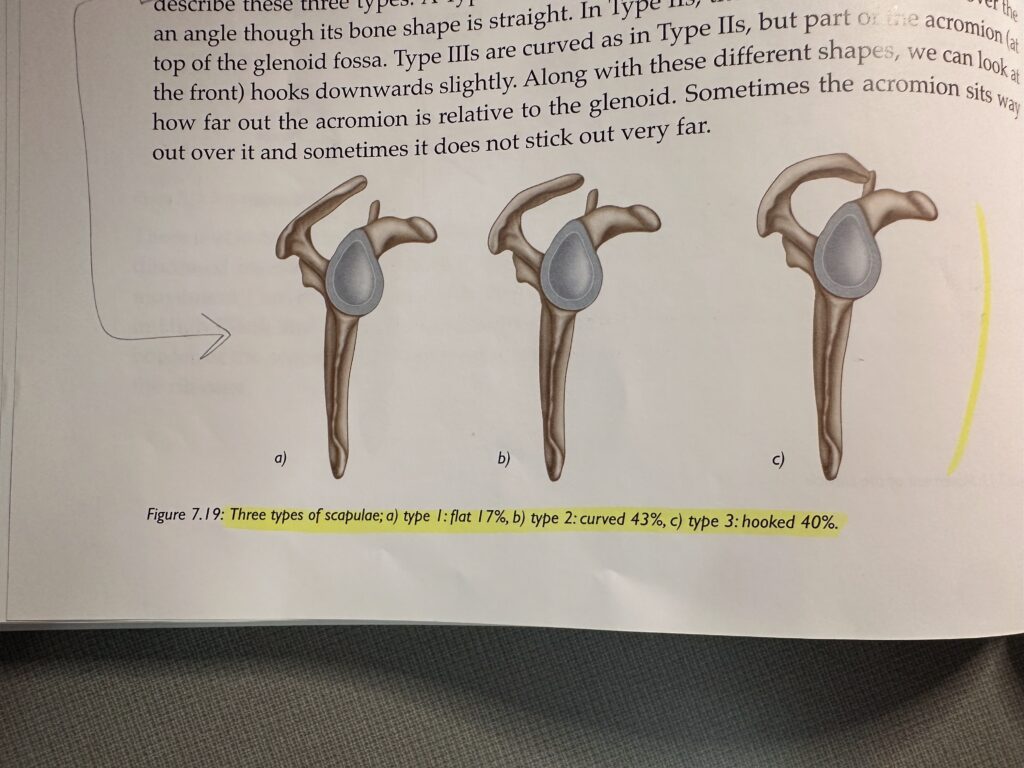
The most common type of scapulae is Type II. Type I acromion can both abduct and flex their arm completely without the scapula moving.
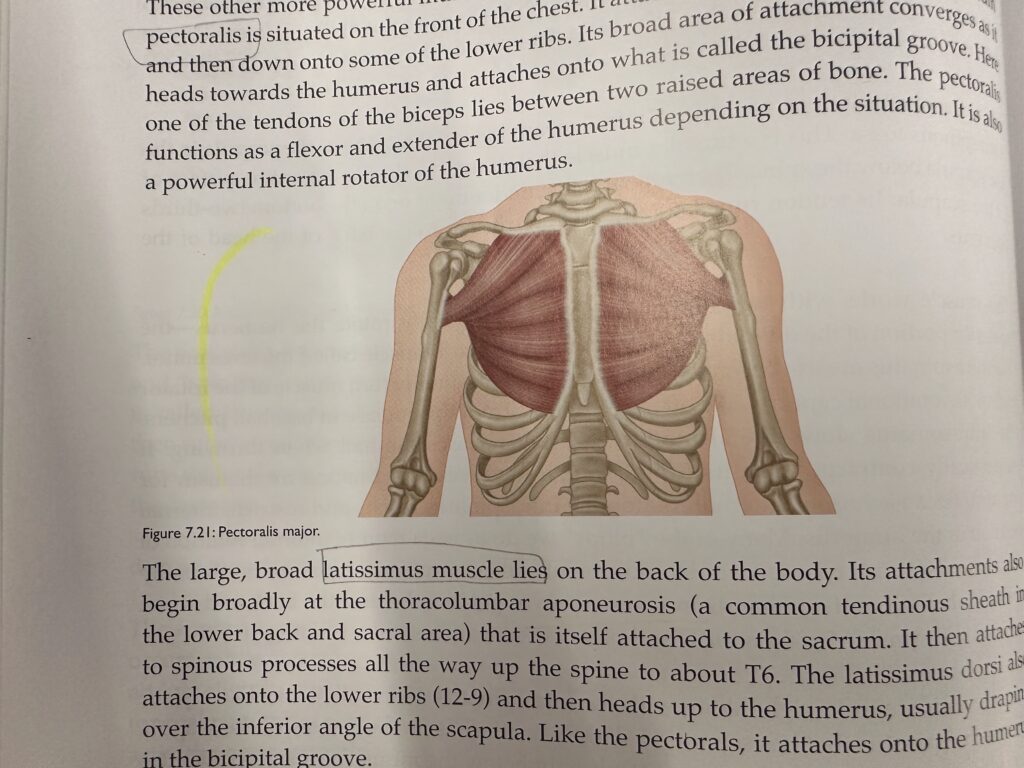
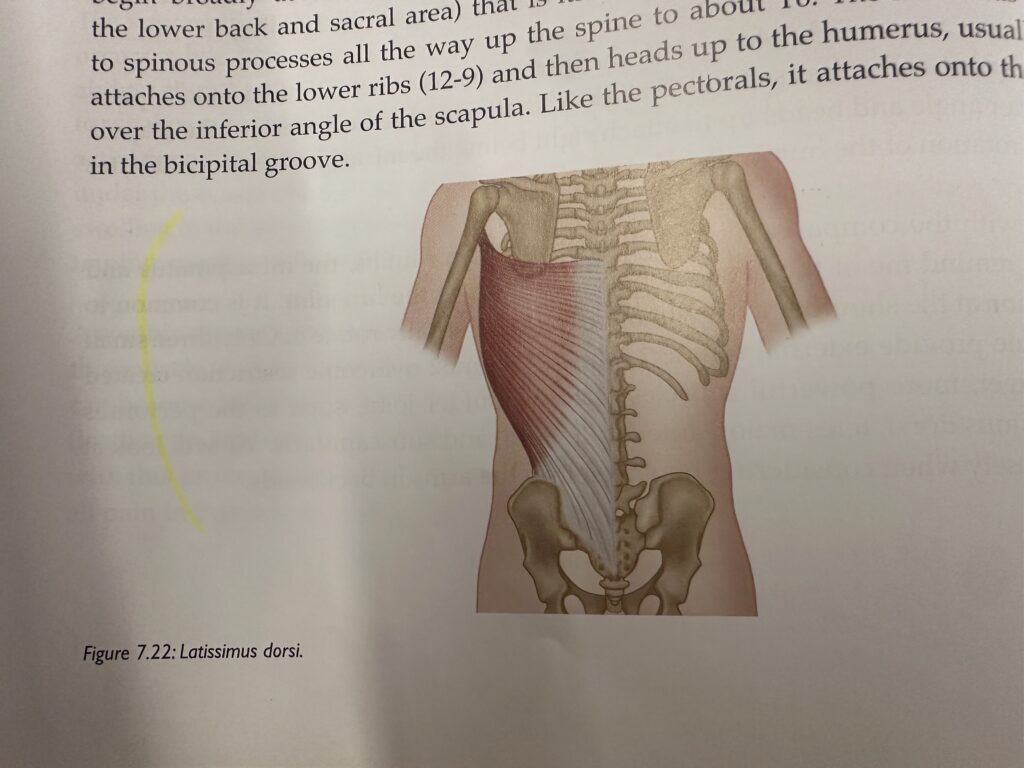
The latissimus dorsi is often well-developed in swimmers. That’s because it’s a powerful internal rotator, extender, and adductor of the humerus – all the actions needed for swimming.
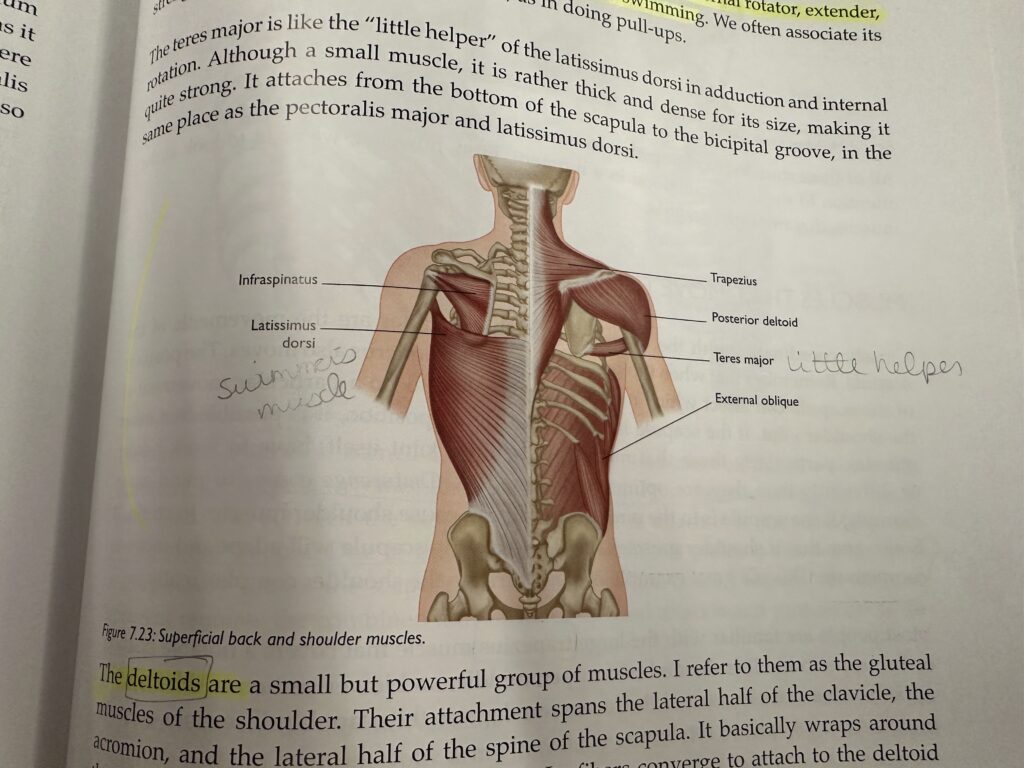
The deltoids are divided into 3 sections – the anterior, middle, and posterior deltoids. The anterior portion assists flexion and internal rotation of the shoulder. The posterior section does the opposite; it assists extension and external rotation. The middle position abducts the shoulder joint.
Closely coordinated with the movements of the shoulder are the movements of the scapula. When the scapula moves, the humerus also moves. The position of the scapula can affect which muscles are recruited to do a particular movement at the shoulder joint.
In Chaturanga, if the scapula is in the wrong place, it can cause shoulder muscles to strain. It is also true that if shoulder muscles are too weak, the scapula will adapt and move to compensate.
The upper section of the trapezius can elevate the scapula, and the lower portion can depress it.
The rhomboids sit between the shoulder blades. They assist in downward rotation and retraction of the scapula.
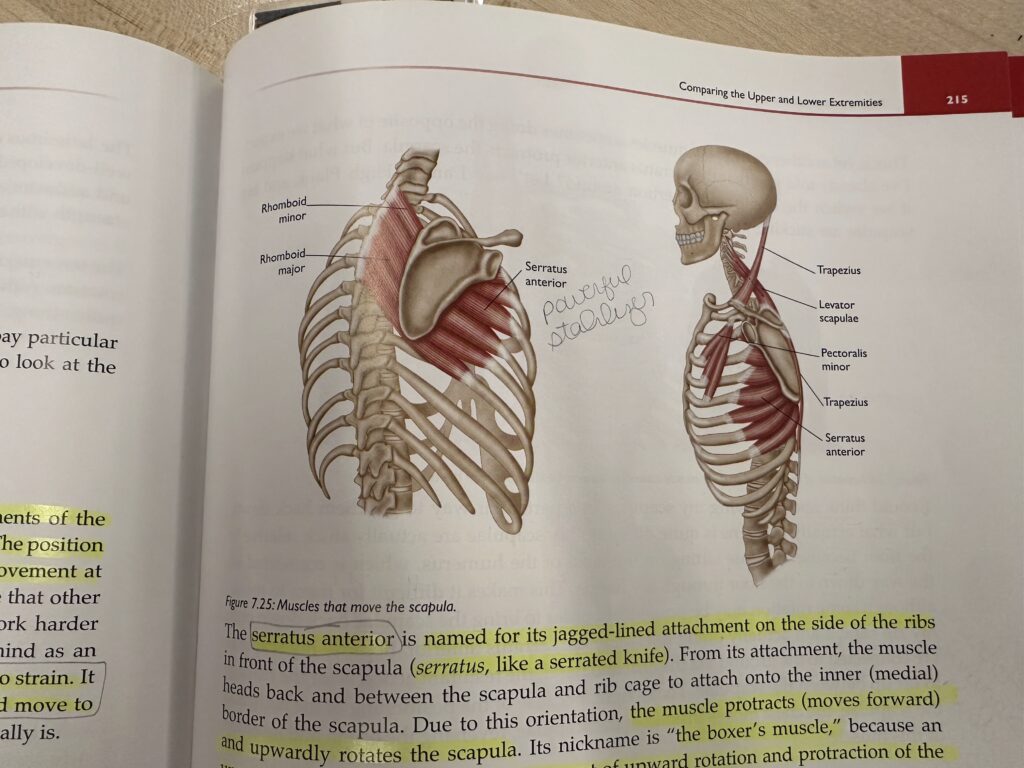
The serratus anterior (serratus like serrated knife) is named for it jagged-lined attachment on the side of the ribs. This muscle moves forward and upwardly rotates the scapula. It’s known as the boxer’s muscle because an uppercut requires the combined movement of upward rotation and protraction of the scapula. It is also a powerful stabilizer of the scapula. If it becomes weak, you can develop a condition known as “winged scapula”. In this the inner border of the scapula will stick up off the back. We often try to avoid this winged position. Even in High Plank or Chaturange, we are susceptibel to the scapulae popping off the back.
If you put your arms into the position for Down Dog, Handstand, Headstand, a forearm balance, or a backbend, you will find that your scapulae are protracted and upwardly rotated.
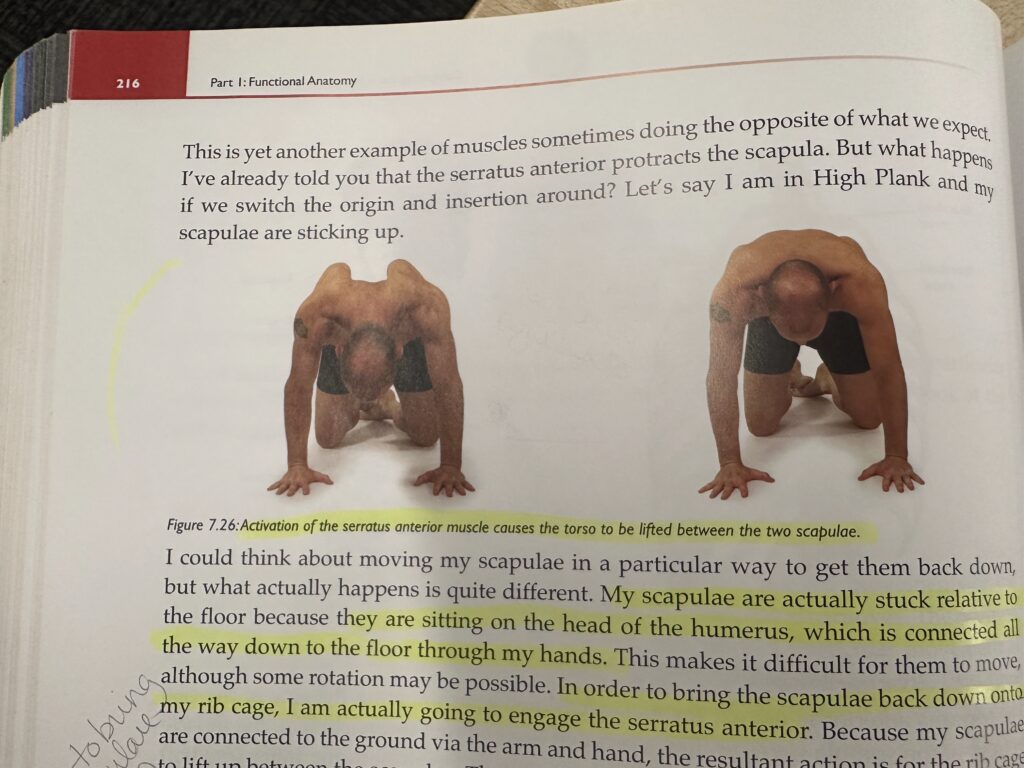
In the above photo, the scapulae are actually stuck relative to the way down to the floor through the hands. In order to bring the scapulae back down onto the rib cage, engage the serratus anterior.
In Chaturanga, the further forward the shoulders are from the hands, the more strain there will be in the shoulders. There are always some exceptions to the rule, but most people will unnecessarily strain their shoulders doing this because they end up too far in front of the hands (The exceptions are usually people with proportionally short upper arms). Most people should have their elbows slightly behind their wrists.
In Upward Facing Dog, people tend to put the shoulder too far in front of the hands and wrists. This puts stress on the wrists and also tends to stress the back as people try to make the back-bending aspect happen. Buttocks may also be tightened for the wrong reasons. Also puts a lit of stress on the shoulders.A risk for the shoulders is when new students practice too much, too soon. This can inflame the shoulders. Depending on the beginner and the style, you may want to simply cut out some Chaturangas. Two basic options for beginners are to put your knees on the floor or to move the hands slightly wider. This allows the larger pec muscles to get involved.
Chapter 8: Hand, Wrist, and Elbow
Changes in hand position not only affect the shoulder joint, but also impact the movement of the scapula.
The middle finger is the centerline of the hand. We’re told to have the middle finger pointing straight forward when the hand is on the floor in yoga postures. For people with tighter shoulders, I often favor using the index finger as the alignment guide.
Most of the powerful muscles that move the hand, fingers, and wrist are actually located on the forearm.
In anatomical position, the palms face forward in supination. If we rotate the palms to face backwards, this is pronation. Pronation and supination of the hand can impact the position of the elbow and shoulder.
Set up yours hands in preparation for Chaturanga. Rotate your fingers so that the index singer is pointing forward, and notice what happens to the hands and elbows. You may find it is easier to keep the elbow in with the hands rotated outwards. Also notice the wrist angle and sensation created when you align your elbows over your wrists. What happens when you move your body back slightly and allow the elbows to sit just behind the line of the wrists.?
General posture and shoulder tension can cause strain as far down as the wrist.
For students suffering with Carpal Tunnel Syndrome, we can help alleviate the tension in their flexor tendons by stretching them, often without bearing weight. Putting the hands in Reverse Prayer position is a great strategy. You can also work with the whole of the shoulder girdle to release tension and/or strengthen areas of it. Work with the micro but don’t forget about the macro if they are in an acute stage of wrist pain.
Chapter 9: Anatomical Patterns in Forward Bends
There will be times when you are working predominantly on strength, times when you are working on flexibility, and times when a posture is all about breath.
By regularly asking ourselves questions, we keep our teaching alive.
Change is a guarantee in life. Remember that things will most certainly change over time.
The most common restriction to forward bending is the hamstrings.
There is a direct fascial relationship connecting the bottoms of the feet to the top of the head. Tension anywhere along this line can create restriction in other areas. Even the feet can impact what a forward bend feels like. If your feet are pulled towards you in dorsiflexion and your toes are extended, you’ll notice a different sensation through the backs of the calves and up your legs.
If you bend your knees, the dynamics and amount of pressure in the hamstrings changes, in addition to your ability to rotate the pelvis. It also allows you to bend further forward. If your hips are tight, the spine has to round more to help bring the head and chest closer to the legs.
An ideal or complete forward bend, where the chest is on the thighs is the result of approximately 2/3 movement at the hip joint and 1/3 movement at the spine.
As you flow through postures in a Sun Salutation, feel the interrelationship of the feet, calves, and hamstrings as they go through the movements of Surya Namaskara. When you arrive in Down Dog, mindfully encourage your heels towards the floor.
In a forward fold, by placing the hips back, you avoid placing pressure on the very muscle that the forward bend is designed to lengthen (the hamstrings). To correct this, you need to bring the hips back in line with the legs.
In Triangle pose, it’s easy to get caught up in the obvious stretch in the front leg. What a revelation it was when the actual sensation of Triangle moved from the hamstrings of the front leg to the outer hip of the back leg.
The opening we feel in the back hip in Triangle is a lengthening of tissues that potentially restrict both hip flexion in a forward bend and hip rotation.
Encourage students doing forward bends with a rounded back to maintain or intend a small amount of arch in their lower back.
When deep in a forward bend, the feet want to twist so that the soles start to face one another. The thighs rotate externally unconsciously to avoid the direct line of tension in the hamstrings. If the legs are straight then there is a more direct line of tension cerated by the hamstrings. We need to work in the opposite direction by internally rotating the thighs.
Tell students that if they need to bend their knees in a pose, once they are in the pose, they should at least try to straighten the knees. Then, use 20 percent of your strength to try and straighten the knees.
If the shoulders are up in the ears with the back of the neck all scrunched up, this pattern tells the teacher the student is relying too heavily on arm strength in their forward bend.
We want to use the hip flexors and quadriceps as much as possible in forward bends.
To elongate the spine in a forward bend, you have to relax the abdominals. If your abs are engaged, the lower back / spine will likely be rounded in flexion.
Naturally we take advantage of our strengths and avoid our weaknesses. This is possibly one of the larger lessons of yoga. Our work is to bring as much balance to our body as we can and to have faith that this will also affect our mind and other habits.
Pay attention to the parts of your anatomy that you tend to avoid. Re-pattern them. These little changes will add up to a nice and simple forward bend.
Chapter 10: Anatomical Patterns in External Hip Rotation
I am all to familiar with the ebb and flow of my ability to do these poses.
Chapter 11: Anatomical Patterns in Twists
Notes
Chapter 12: Anatomical Patterns in Arm Balances
Notes
Chapter 13: Anatomical Patterns in Backbends
Notes
Online Anatomy Course
Anything facing the midline of the body is considered medial. Anything facing outward form that midline is lateral.
For two ends of a bones, the closer end to the head is considered proximal, the end further away is called distal.
All movement happens at the joints, bones just follow.
Anterior = front, Posterior = back.
Superior = on top of, Inferior = below.
Flexion = decreasing the angle of the joint. Also is moving of a joint away from anatomical position.
Extension = increasing the angle of the joint. Also is moving of a joint back to anatomical position.
Abduction = movement away from the plane that splits the body left to right
Adduction = movement back towards plane that splits the body left to right
Smooth muscles are found in the stomach, intestines, and blood vessels, cardiac muscles are found in the heart, and skeletal muscle is found everywhere else.
Blood cells that are in our body are generated and come out of our bones.
When in a warrior pose, if the knee is bent inwards, try and lift the toes to engage the arches. This should ever so slightly nudge the laterally to get it to face more forward. Then keep the knee there and place the toes back down.
When trying to do triangle, first bend the knee to get it pointing forward, then move hands into position, then straighten the knee.
Other Notes
Notes
@joekotlan on X